Ever had a patient complain about restless sleep, fatigue, or unexplained movements during the night? Chances are, you’ve encountered Periodic Limb Movement Disorder (PLMD). While it often flies under the radar, PLMD treatment is crucial for improving sleep quality and overall well-being.
In this guide, we’ll dive deep into what PLMD is, why treatment matters, and explore both conventional and advanced approaches. We’ll also share real-world examples and highlight professional strategies for long-term management.
What is PLMD (Periodic Limb Movement Disorder)?
PLMD is a sleep disorder characterized by involuntary, repetitive leg movements during sleep. These movements often last 0.5–10 seconds and occur every 20–40 seconds throughout the night.
Unlike Restless Legs Syndrome (RLS), PLMD doesn’t always involve an urge to move the legs while awake. Instead, the movements typically disturb sleep, leading to daytime fatigue, poor concentration, and irritability.
Common Symptoms of PLMD
Sudden, jerking leg movements during sleep
Bed partner complaints of “kicking” or “twitching”
Insomnia or frequent nighttime awakenings
Daytime drowsiness and low energy levels
How PLMD Differs from Restless Legs Syndrome (RLS)
Although they sometimes coexist, RLS and PLMD are different:
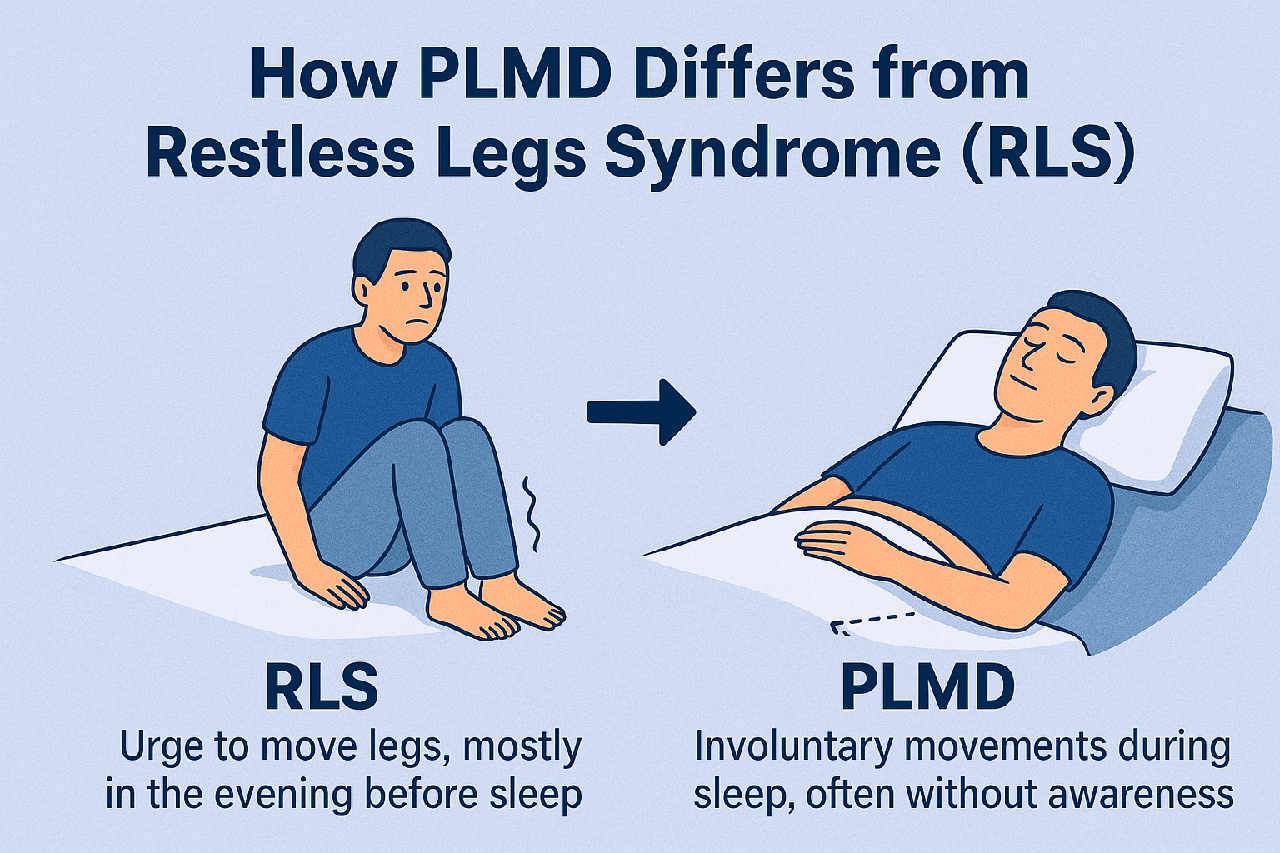
RLS → Urge to move legs, mostly in the evening before sleep.
PLMD → Involuntary movements during sleep, often without awareness.
👉 This distinction is key for professionals when choosing the right PLMD treatment plan.
Why Timely Treatment for PLMD Matters
Impact on Sleep Quality
Left untreated, PLMD leads to fragmented sleep, which translates to poor rest and reduced productivity during the day.
Cognitive and Physical Consequences
Over time, PLMD contributes to:
Memory problems
Decreased focus
Higher risk of accidents due to daytime sleepiness
Emotional instability
Clearly, early intervention in PLMD treatment is essential.
Diagnosis: The First Step in PLMD Treatment
Before treatment, professionals must ensure accurate diagnosis.
Role of Polysomnography (Sleep Study)
Polysomnography records brain waves, breathing, heart rate, and limb movements during sleep. It remains the gold standard for PLMD diagnosis.
Clinical Evaluation & Patient History
Detailed history-taking helps rule out RLS, sleep apnea, or medication-induced movement disorders, ensuring precise treatment planning.
Conventional PLMD Treatment Options
Medication-Based Approaches
Dopaminergic Agents
Drugs like pramipexole and ropinirole are often prescribed, though they carry a risk of long-term tolerance and augmentation.
Anticonvulsants
Gabapentin and pregabalin help reduce nerve excitability, improving sleep quality in patients with PLMD.
Benzodiazepines & Sedatives
Clonazepam may be used in severe cases, but caution is needed due to dependency risks.
Non-Medication Approaches
Lifestyle Adjustments
Reducing caffeine, alcohol, and nicotine can make a noticeable difference.
Sleep Hygiene
Maintaining a consistent bedtime routine, optimizing sleep environment, and limiting screen time are highly recommended.
Exercise & Stress Management
Gentle stretching, yoga, and relaxation techniques lower nighttime movement frequency.
Emerging & Advanced PLMD Treatments
Neuromodulation Techniques
Research is exploring transcranial magnetic stimulation (TMS) and other non-invasive methods to regulate neural activity.
Role of Cognitive Behavioral Therapy (CBT-I)
CBT for insomnia, combined with medical care, addresses behavioral triggers that worsen PLMD symptoms.
Personalized Treatment Plans
Combining pharmacological and non-pharmacological therapies tailored to patient history yields the best results.
Integrative & Alternative Therapies
Nutritional Support
Iron supplementation (for low ferritin levels)
Magnesium for muscle relaxation
Vitamin B12 for nervous system support
Herbal Remedies & Natural Approaches
Chamomile tea, valerian root, and melatonin are being explored as complementary aids.
Case Examples: How Patients Respond to PLMD Treatment
Case Study 1: Medication + Lifestyle Adjustment
A 52-year-old man experienced reduced limb movements after starting gabapentin, along with cutting caffeine and sticking to a sleep schedule.
Case Study 2: Advanced Therapy Integration
A 40-year-old woman with persistent PLMD found relief through a combination of dopaminergic medication and CBT-I, significantly improving her quality of life.
Challenges in Treating PLMD
Misdiagnosis with RLS
Because symptoms overlap, some patients are mistakenly treated for RLS, delaying proper care.
Long-Term Medication Concerns
Tolerance, side effects, and dependency remain pressing issues for professionals managing PLMD.
Preventive Measures & Long-Term Management
Routine sleep assessments every 6–12 months
Regular monitoring of iron and vitamin levels
Ongoing professional follow-ups to adjust treatment plans
FAQs About PLMD Treatment
Q1. Can PLMD be cured permanently?
Currently, there’s no permanent cure, but treatments can significantly reduce symptoms.
Q2. What’s the most effective medication for PLMD?
Dopaminergic agents like pramipexole often work well, but treatment must be personalized.
Q3. Is PLMD linked to mental health issues?
Yes, untreated PLMD can worsen anxiety, depression, and cognitive decline.
Q4. Can lifestyle changes alone manage PLMD?
For mild cases, yes. But moderate to severe cases usually require combined treatment.
Q5. How is PLMD diagnosed?
Through polysomnography (sleep study) and detailed clinical history.
Q6. Is PLMD common in children?
Yes, though less studied. Pediatric cases are often linked to iron deficiency.
Conclusion: A Holistic Path to PLMD Relief
Treating PLMD isn’t about a one-size-fits-all solution. Instead, it’s a blend of medical treatment, lifestyle modification, and professional follow-up.
For professionals, staying updated on both conventional and emerging PLMD treatments ensures better patient outcomes and long-term relief.
👉 If you’re a healthcare provider, consider integrating both clinical expertise and holistic approaches to manage PLMD effectively.
For more on sleep-related disorders, check out resources from the American Academy of Sleep Medicine.